Last Updated on June 19, 2025 by Lauretta Iyamu, PharmD
You feel a strange numbness in your hand that won’t go away.
Or your vision blurs for no reason.
It’s easy to brush these early signs and symptoms of MS off, but what if they’re your body’s early warning signs?
Multiple sclerosis affects nearly 3 million people worldwide, and yet many are diagnosed years after their first symptoms begin.
Why, you may ask?
It is because these early signs and symptoms of MS are often easy to miss and are frequently dismissed.
But here’s what most people don’t realize: early diagnosis makes a difference.
The sooner multiple sclerosis (MS) is detected, the sooner treatment can begin and the better the long-term outlook.
If you’ve been wondering about odd neurological symptoms or if MS runs in your family, this guide will walk you through he early signs and symptoms of MS, its diagnosis, what to look for, when to act, and how to protect yourself.
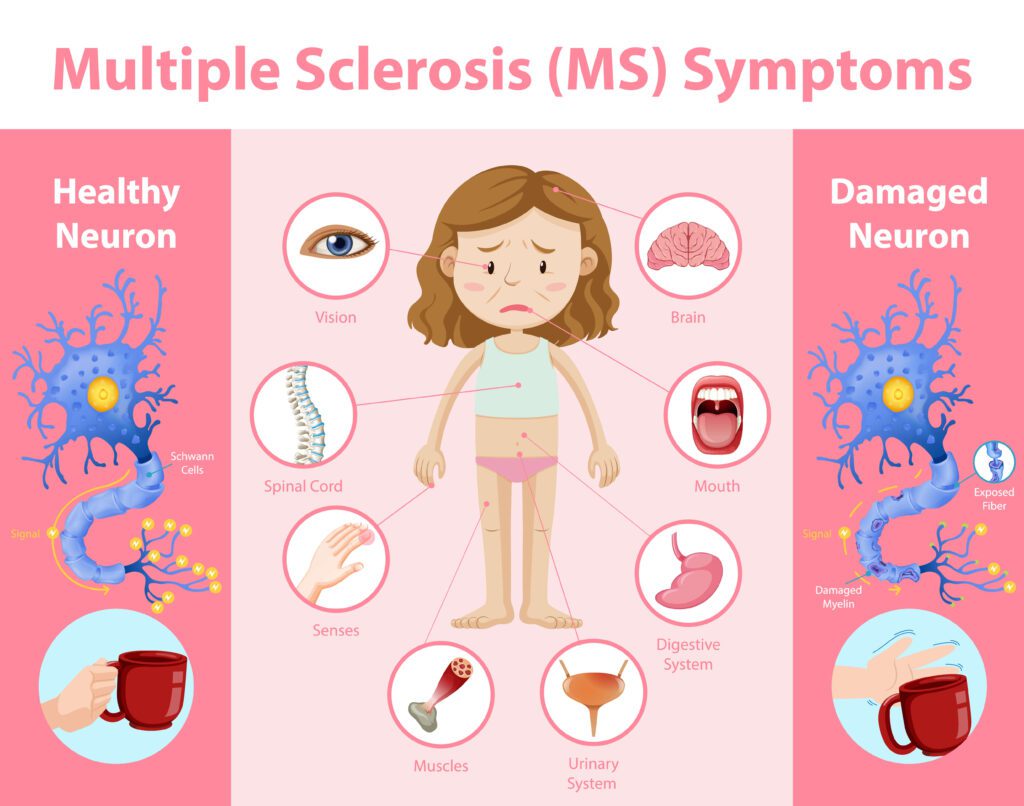
What is Multiple Sclerosis?
Multiple sclerosis (MS) is a long-term, autoimmune condition that affects your central nervous system, including the brain and spinal cord.
Your immune system, which usually fights off infections, mistakenly attacks the protective coating around your nerves.
This coating is called myelin.
Once it’s damaged, signals from your brain slow down or get lost.
That’s what causes MS symptoms.

According to a study review published in the European Journal of Neurology, MS is the most common non-traumatic disabling disease to affect young adults.
Here’s what makes MS unique:
- It doesn’t follow one clear pattern.
- It can start mild and then worsen.
- It often comes and goes; symptoms may appear, disappear, and then return [2].
There are four main types of MS:
- Relapsing-Remitting MS (RRMS): The most common. Symptoms flare, then ease up.
- Primary Progressive MS (PPMS): Steady symptoms that get worse over time.
- Secondary Progressive MS (SPMS): Initially relapsing, then progresses to a more consistent pattern.
- Clinically Isolated Syndrome (CIS): A single episode of MS-like symptoms.
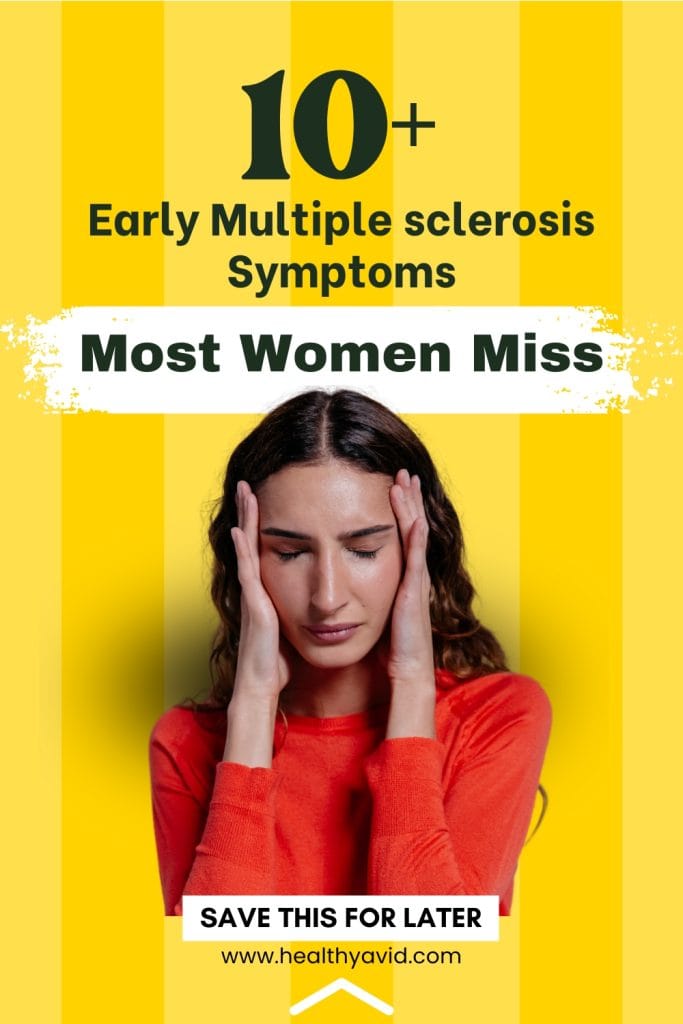
MS tends to strike in your 20s to 40s, but it can happen earlier or later.
Women are two to three times more likely than men to develop it.
Why does catching it early matter?
Because nerve damage adds up over time.
The longer MS goes untreated, the harder it becomes to slow or manage.
Early Signs and Symptoms of Multiple Sclerosis
Most people think multiple sclerosis begins with something dramatic.
But it usually doesn’t
MS often starts with minor symptoms that seem harmless at first.
You might think you’re just tired, stressed, or aging.
But these early signs matter.
They are your body’s way of warning you that something’s wrong with your nervous system.
When you know what to look for, you can act sooner, and that can make a big difference.
Here are the most common early symptoms and symptoms of MS, explained in simple terms [3, 4].
Common signs and symptoms of multiple sclerosis:
- Vision problems
- Numbness and Tingling
- Fatigue
- Muscle Weakness and Spasms
- Difficulty Walking
- Cognitive Changes
- Chronic Pain
- Bladder and Bowel Issues
- Dizziness and Vertigo
- Mood changes
1. Vision Problems

MS can cause swelling in the nerve that connects your eye to your brain.
That’s called optic neuritis.
It can make you see things in a different way [4].
You may notice:
- Blurry or hazy vision
- Double vision (seeing two images at once)
- Pain behind your eye, especially when you move it
- Colors look faded or wrong
Some people experience a temporary loss of vision for a few days or weeks.
This can be scary, but with treatment, it often improves.
Vision problems are often one of the early signs and symptoms of multiple sclerosis (MS).
2. Numbness and Tingling

One side of your face feels weird.
Or your fingers go numb out of nowhere.
Maybe your legs feel like they’re buzzing, like they’ve “fallen asleep.”
These are all common early signs and symptoms of MS.
The nerves in your body send signals to your brain.
When MS causes damage to those nerves, those signals get messed up.
These sensations caused by nerve damage can range from mild to severe [5].
That’s why you might feel:
- Tingling
- Pins and needles
- Loss of feeling
- A feeling like ants crawling on your skin
Areas Prone to Numbness
- Face
- Arms
- Legs
- Fingers
It usually happens on one side.
It may go away and then return.
That’s a red flag.
3. Extreme Fatigue That Doesn’t Go Away
This isn’t just feeling tired.
It’s a deep, heavy kind of tired that doesn’t match what you’ve done that day.
It can show up even if you slept well.
Signs of MS-Related Fatigue:
- Makes it hard to focus
- It can come on suddenly
- Doesn’t get better with rest
- Feels like your body is shutting down
- Feeling tired every day
- Triggered by heat and humidity
- Getting worse as the day goes on
Many people with early MS say fatigue was their first real clue, but they thought they were just overworked.
It can make daily activities very difficult [6].
Don’t ignore it if the issue persists.
4. Muscle Weakness and Spasms
You used to climb stairs easily.
Now your legs feel heavy.
You try to hold something, and your hand doesn’t cooperate.
This weakness isn’t from working out too hard.
This happens because MS damages the nerve fibers that stimulate your muscles.
This can make moving and doing everyday tasks hard [7].
According to the National Multiple Sclerosis Society, up to 60 percent of people with MS have muscle weakness in their arms, legs, or faces.
You may feel:
-
Signs of Muscle Issues
-
Stiff or tight muscles
-
Sensitivity to heat or cold
-
Weakness in arms or legs
-
Uncontrolled muscle movements
-
Dropping things more often
- Legs that “give out” without warning
This is how MS often affects mobility in its early stages.
5. Difficulty Walking
You’re walking in a straight line and suddenly feel like you’re tipping over.
You reach for something and nearly fall.
It’s not clumsiness.
It’s not old age.
It’s your brain having trouble coordinating movement.
Early MS often affects balance and coordination.
This might be due to muscle weakness, stiffness, or dizziness [8].
You might notice:
- Feeling off-balance
- Trouble walking in the dark
- Falling more than usual
- Feeling dizzy when you turn your head
- Dragging one leg
If this keeps happening, don’t ignore it.
6. Cognitive Changes
Do you keep losing your train of thought?
Struggling to follow conversations?
These might seem like small things, but they can be part of early MS.
The brain fog many people with MS describe is very real.
You may notice:
- Forgetting what you were doing
- Struggling to find the right word
- Slower thinking than usual
- Trouble focusing on one task
- Difficulty organizing or planning
It’s frustrating.
And it’s not “just stress” if it’s happening often.
These early signs are your body’s way of speaking to you.
Not everyone will have all of these symptoms.
Some may come and go.
Some may seem unrelated.
But if you’re noticing more than one, or they’re happening more often, it’s time to talk to your doctor.
The sooner MS is caught, the more can be done to slow it down.
These issues can affect your ability to think clearly and solve problems [9].
Other Early Warning Signs of MS That Are Often Overlooked
Not all MS symptoms are noticeable.
Some signs are easy to explain away until they start adding up.
These subtle signals can appear months or even years before diagnosis.
If you’re paying attention now, you can catch MS earlier and start protecting your nervous system.
Here’s what to look for:
7. Heat Sensitivity
Do your symptoms get worse in warm weather?
This is known as Uhthoff’s phenomenon, and it’s common in multiple sclerosis (MS).
Even a slight rise in body temperature can temporarily:
- Blur your vision
- Slow your thinking
- Make you feel weak
- Worsening numbness or tingling
It’s not dangerous, but it’s a clear sign your nerves are struggling to keep up.
8. Bladder and Bowel Changes
Needing to pee constantly?
Can’t hold it in?
Straining to go?
These are early signs of neurogenic bladder, where MS begins to affect the nerves that control urination and bowel movements.
In MS, this can lead to:
- Urgency (gotta go NOW)
- Frequency (going more than usual)
- Incontinence (leaks before you get there)
- Constipation or incomplete emptying
These symptoms may be mild at first, but if you’re otherwise healthy, they’re worth checking out [11].
9. Sexual Dysfunction
For women, it might feel like numbness, dryness, or a total loss of desire.
For men, it might show up as erectile dysfunction or reduced sensation.
This happens because MS can interrupt the nerve signals between the brain and sexual organs.
It’s not “just stress” or hormones, especially if it’s sudden or unexplained.
10. Mood Swings and Depression
Emotions out of balance?
Crying easily?
Feeling flat or unusually irritable?
MS doesn’t just affect your body; it affects your brain chemistry, too.
Mood changes can show up before other signs.
These include:
- Depression that doesn’t match your life situation
- Anxiety that seems new or intense
- Quick mood shifts without a clear cause
- Feeling emotionally “off” or out of control
If this is happening alongside other neurological symptoms, don’t dismiss it.
Speak with your doctor to get treatment for both conditions as soon as possible.
11. Speech Problems
You know what you want to say, but it’s not coming out right.
This can include:
- Slurred speech
- Slowing down when talking
- Pausing to find the right words
- Saying words out of order
These symptoms are easy to ignore, but if they keep coming back, they could be early signs of MS.
12. Dizziness or Vertigo
It might feel like the room is spinning.
Or you suddenly lose your sense of balance.
Or you’re walking like you’re on a boat.
This isn’t “just dehydration” or “standing up too fast.”
If it keeps happening, it may be your brain’s balance center being affected by MS.
These are quiet symptoms.
They don’t shout, but they matter.
These can make it hard to keep your balance [12].
Especially if you’re experiencing more than one.
If you’re noticing strange changes in your body that you can’t explain, listen to that voice inside.
Early MS is subtle, but it speaks if you’re paying attention.
Signs of Dizziness and Vertigo
- Feeling lightheaded
- Room spinning sensation
- Loss of balance
13. Chronic Pain
Chronic pain is another early symptom of MS.
This pain can be caused by nerve damage or muscle stiffness and spasms [10].
Types of MS-Related Pain
- Burning or tingling pain (neuropathic pain)
- Joint or muscle pain (musculoskeletal pain)
MS Symptoms by Body System
Multiple sclerosis affects different parts of your body depending on which nerves are under attack.
Here’s how MS symptoms show up system by system, so you can better recognize what’s happening.
1. Neurological System
This is the core of MS, because MS is a neurological disease.
Common symptoms:
- Tremors – uncontrollable shaking, usually in hands or arms
- Spasticity – muscles feel stiff or tight, especially in the legs
- Seizures – rare, but possible if MS lesions irritate certain brain areas
- Nerve pain – sharp, stabbing, or burning sensations with no apparent cause
These signals mean your nerves are misfiring or struggling to fire at all.
2. Visual System
The optic nerves are often among the first affected by MS.
Watch for:
- Blurred vision in one eye
- Double vision
- Pain behind the eye, especially when moving the eye
- Color vision changes, especially red and green, look faded
This is often caused by optic neuritis, a common early symptom that can be temporary but serious.
3. Motor System (Movement and Muscles)
MS makes it harder for the brain to send clear signals to your muscles.
This shows up as:
- Muscle weakness
- Dragging a foot when walking
- Trouble with coordination
- Sudden muscle spasms
- Difficulty using your hands or opening jars
These symptoms may initially come and go, but they often recur.
4. Sensory System (Touch and Feel)
This is one of the most common ways MS first shows up.
You might notice:
- Numbness or tingling in the face, hands, feet, or legs
- Burning or stabbing sensations
- A tight “band” feeling around your torso (called the “MS hug”)
- Hypersensitivity to touch or cold
These odd sensations are caused by damaged sensory nerves, not your imagination.
5. Cognitive Function (Thinking and Memory)
Even in its early stages, MS can impact your cognitive function.
You may notice:
- Slower thinking or processing
- Trouble focusing on tasks
- Difficulty finding words
- Memory lapses, forgetting recent events or plans
These are part of MS cognitive dysfunction, and they can be very frustrating, especially when you “feel fine” otherwise.
6. Emotional Regulation
MS can disrupt mood and emotional control.
This can include:
- Mood swings
- Uncontrollable laughter or crying (pseudobulbar affect)
- Feeling emotionally numb or disconnected
It’s not “just stress.”
Your brain’s emotional centers can be affected by inflammation and nerve damage, too.
When you see how these symptoms connect across your body, it’s easier to understand how MS works.
Knowing these patterns helps you speak up early, get the proper tests, and protect your brain and body.
Risk Factors of Multiple Sclerosis
Women are more likely to get MS than men, with about three women getting MS for every man who does [5].
Several environmental factors and lifestyles may increase your exposure to MS [3].
Here are some factors that can increase your risk of getting MS [6]:
- Not Enough Vitamin D or Sunlight
- Epstein-Barr virus (EBV)
- Infection
- Obesity
- Smoking
- Family History
1. Genetics and Family History
If family members have MS, your risk is higher.
But it’s not a guarantee.
It’s about watching for signs early and acting fast.
2. Sunlight and Vitamin D
Low vitamin D has been linked to MS.
Safe sunlight and supplements can help.
Ask your doctor for the correct dose based on your lab results.
3. Smoking
Tobacco use increases the risk and severity of MS.
Quitting now can reduce future damage, even after diagnosis.
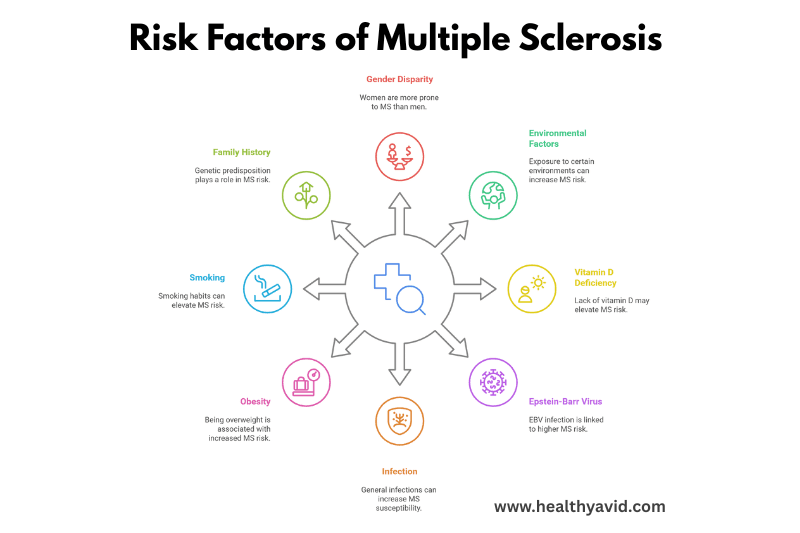
4. Obesity and Diet
Extra weight stresses your immune system.
Eating a healthy diet, staying active, and maintaining a healthy weight can help reduce inflammation.
5. Viral Infections
Viruses like EBV (Epstein-Barr) have been linked to MS risk.
Protect yourself with good hygiene and vaccination when possible.
Is MS Hereditary?
The chance of having MS occurs throughout life, starting in the womb.
Your genetic makeup influences your risk of MS if you have a family history of the disease, as well as environmental factors [3].
When you have a first-degree relative with multiple sclerosis, your risk of developing MS is around 5% to 25%.
If you’re an identical twin, there is a higher chance of this condition being present in your family history [6].
For example, you may find that when MS affects an identical twin, one twin can have mild MS that comes and goes, while the other’s condition may be more severe with serious long-term effects [6].
Other Conditions That Look Like MS (Comorbid Disorders)
Not every symptom points to MS.
Sometimes it’s something else entirely.
But early on, many conditions overlap.
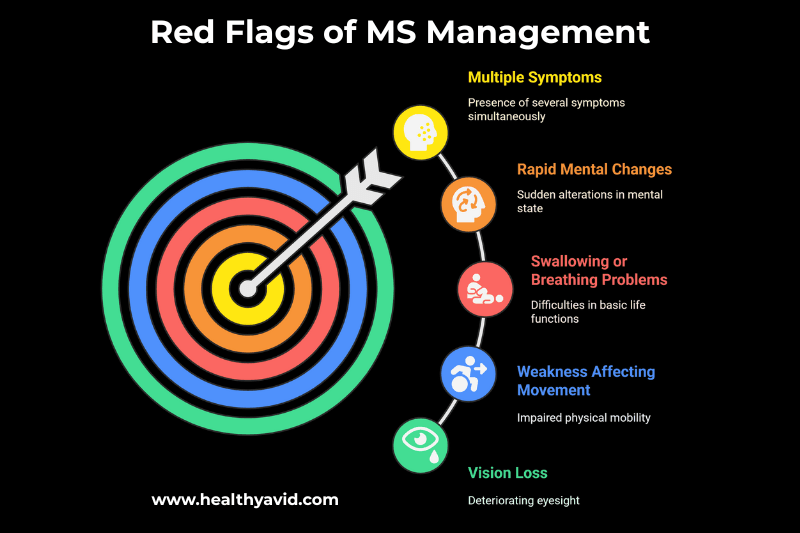
These are significant red flags to look for in MS, including comorbid symptoms and signs.
These signs help your doctor differentiate multiple sclerosis (MS) from other autoimmune diseases with similar signs and symptoms[7], [8].
Examples of comorbid autoimmune disorders:
- Systemic lupus erythematosus
- Sjögren’s disease
- Behçet’s disease
- Susac’s disease
- Other vasculitides
- Lyme disease
- HIV
- Parkinson’s disease
- Rheumatoid Arthritis
- Alzheimer disease
- Inflammatory bowel disease
Here’s how to tell them apart.
1. Vitamin B12 Deficiency
B12 is key for healthy nerves. Low B12 can cause:
- Fatigue
- Numbness or tingling
- Weakness
- Balance problems
That sounds like MS, right?
But a simple blood test can check your B12 levels.
If it’s low, supplements can help, not MS treatments.
2. Lyme Disease or Other Infections
Sometimes infections like Lyme can mimic MS almost exactly.
They can cause:
- Joint pain
- Nerve problems
- Vision changes
- Brain fog
Doctors often use blood tests and a patient’s medical history to identify these infections.
Treating the disease can reverse symptoms, unlike MS, which is chronic.
3. Autoimmune Diseases
Conditions like lupus and rheumatoid arthritis also affect the immune system.
They can share symptoms with MS, such as:
- Fatigue
- Joint and muscle pain
- Nerve symptoms
Doctors will do blood tests for specific markers (like ANA or rheumatoid factor) to pinpoint the cause.
4. Migraines and Tension Headaches
Migraines can cause:
- Tingling
- Altered vision (aura)
- Numbness
- Confusion
They can feel very similar to MS at first.
But headaches tend to come with severe pain and have a distinct rhythm.
A neurologist can help determine whether it’s a migraine or something more serious.
5. Anxiety and Stress Disorders
Stress and anxiety can cause:
- Brain fog
- Muscle weakness
- Fatigue
- Tension
However, with stress alone, other physical signs, such as optic neuritis or numbness, typically don’t occur.
Tracking your symptoms in a diary and consulting with your healthcare provider can help clarify the cause.
How to Diagnose Multiple Sclerosis

There is no single, defined test for multiple sclerosis.
Your doctor will only diagnose you with MS after ruling out other diseases or comorbid disorders that might be causing your symptoms.
The diagnosis of multiple sclerosis remains clinical.
However, once all the signs and symptoms of MS are known, you will get one of the following diagnoses:
1. Differential diagnosis
A differential diagnosis is when your doctor distinguishes between two or more conditions that could be causing your symptoms.
2. Diagnosis of exclusion
A diagnosis of exclusion occurs when your doctor diagnoses a condition by eliminating other possibilities.
This occurs because they could not confidently determine the cause of your symptoms based on your history, examination, or test results.
Diagnostic Tests for MS
Doctors use several tests to diagnose multiple sclerosis (MS).
These tests help rule out other conditions and confirm a diagnosis of multiple sclerosis (MS) [14].
Common Diagnostic Tests
- Blood test
- Medical history
- Physical examination
- MRI scans to look for lesions in the brain and spinal cord
- Lumbar puncture (spinal tap) to check cerebrospinal fluid
- Evoked potentials to measure electrical activity in the brain
1. Your Story and Physical Exam
Expect questions like:
- When did symptoms start?
- How long did they last?
- Any vision or balance changes?
Then they’ll check how your nerves work:
- Your reflexes
- Muscle strength
- Coordinate tests
- Eye movement
- Sensation tests
2. MRI of the Brain and Spine
MRI scans are the gold standard.
They look for areas of damage in your central nervous system.
Lesions alone aren’t proof of MS.
But when combined with symptoms, they point the way.
3. Lumbar Puncture (Spinal Tap)
Doctors may test your cerebrospinal fluid to look for:
- Immune markers
- Oligoclonal bands
These indicate the kind of inflammation seen in MS.
Not everyone needs one, but it can aid in diagnosis.
4. Blood Tests
These rule out other conditions. They often test for:
- B12 levels
- Autoimmune markers (like ANA or rheumatoid factor)
- Lyme disease
- Other infections
5. McDonald Criteria
This is a checklist doctors use.
It combines your symptoms, test results, and lesion locations to make an official diagnosis of multiple sclerosis (MS) [13].
Preparing for Your Appointment
- Keep a diary of your symptoms
- List any medications and supplements you take
- Note any family history of autoimmune diseases
Living with Early MS (What to Do Now)
Early detection empowers you to act.
Here’s what comes next:
1. Build Your Healthcare Team
You’ll probably work with:
- A neurologist
- A nurse specialist
- A rehab therapist
- A mental health counselor
They’ll create a plan tailored to your needs.
2. Medications
Some medicines can help manage MS symptoms and slow down the disease.
These include disease-modifying therapies (DMTs), steroids for acute relapses, and medications to manage specific symptoms like muscle spasms or pain [15].
Types of Medications for Multiple Sclerosis
- Corticosteroids
- Muscle relaxants
- Disease-modifying therapies (DMTs)
These include:
- Injectables
- Oral medications
- Infusions
Early treatment means better long-term control.
3. Healthy Lifestyle Habits
This includes:
- Balanced diet
- Regular exercise
- Good sleep
- Stress management
- Vitamin D
These steps support treatment and improve daily life [16].
4. Join a Support Network
Living with MS can feel lonely.
Therapy and support groups offer both emotional and practical support.
You’ll meet people who get it.
Technology and Tools for Tracking Symptoms of MS
Modern tools make managing MS easier:
- Apps: to track symptoms, meds, fatigue
- Wearables: track steps, sleep, balance
- Telemedicine: online consults save energy
- Brain games: help with cognitive rehab
These tools help you stay on top of changes and treatment.
Diet and Supplements for MS
While there is no single “MS diet,” specific dietary patterns and principles are generally recommended to support overall health and potentially manage MS symptoms.
These include:
1. Anti-Inflammatory Diet:
Eating foods known to reduce inflammation, such as fruits, vegetables, whole grains, lean protein, and healthy fats (omega-3 fatty acids).
Limiting processed foods, refined sugars, and saturated/trans fats.
2. Mediterranean Diet:
A well-studied dietary pattern rich in fruits, vegetables, olive oil, fish, and whole grains.
It aligns with anti-inflammatory principles and has been associated with various health benefits.
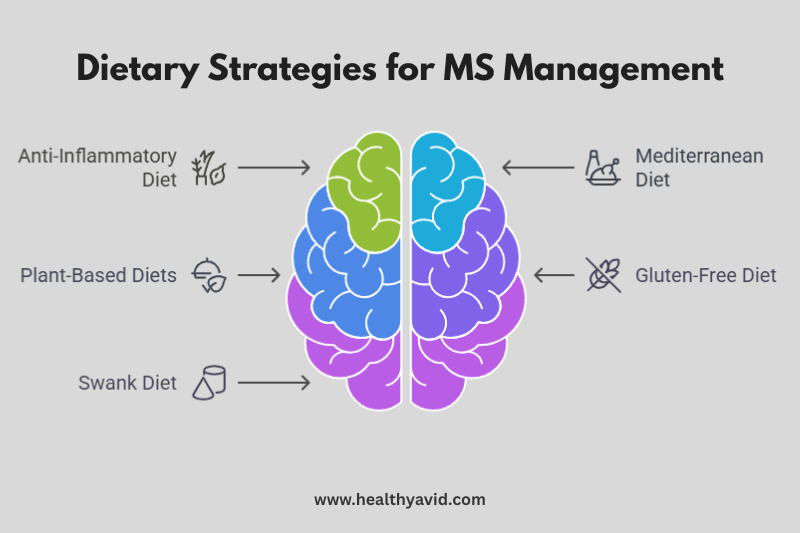
3. Plant-Based Diets:
Vegetarian and vegan diets can be beneficial due to their high content of fruits, vegetables, and fiber.
However, careful planning is necessary to ensure an adequate intake of essential nutrients, such as vitamin B12, iron, and calcium.
4. Gluten-Free Diet:
Some individuals with MS report symptom improvement on a gluten-free diet.
However, there is limited scientific evidence to support this for the general multiple sclerosis (MS) population.
Always consult with a healthcare professional before eliminating gluten to rule out other potential causes of symptoms.
5. Swank Diet:
This diet, developed by Dr. Roy Swank, is a low-fat diet that restricts saturated fat intake.
Some studies suggest it may slow the progression of MS, but more research is needed.
Specific Nutrients and Supplements
Several nutrients and supplements have been investigated for their potential role in managing multiple sclerosis (MS) [18].
These include:
1. Vitamin D:
Low vitamin D levels are common in people with MS and have been linked to increased disease activity.
Supplementation may be beneficial, but optimal dosage should be determined by a healthcare provider based on individual needs and blood levels.
2. Omega-3 Fatty Acids:
Found in fatty fish, flaxseed, and walnuts, omega-3 fatty acids have anti-inflammatory properties and may help reduce MS symptoms.
3. B Vitamins:
Vitamins B12 and folate are needed for nerve health.
Vitamin B12 deficiency is common in people with MS, especially those taking certain medications.
4. Antioxidants:
Vitamins C and E, as well as selenium and coenzyme Q10, are antioxidants that may help protect against oxidative stress, a condition implicated in multiple sclerosis (MS).
5. Probiotics:
These beneficial bacteria may support gut health and immune function, which could indirectly benefit individuals with multiple sclerosis (MS).
6. Alpha-Lipoic Acid (ALA):
An antioxidant that may have neuroprotective effects. Some studies suggest it may slow the progression of MS, but more research is needed.
7. Biotin:
High-dose biotin has been investigated as a potential treatment for progressive MS, with some studies showing promising results.
However, it can interfere with certain lab tests, so please inform your doctor if you are taking it.
Considerations and Cautions
1. Individualized Approach:
Dietary and supplement needs vary depending on individual factors such as disease stage, symptoms, medications, and overall health.
2. Consultation with Healthcare Professionals:
It is crucial to consult with a neurologist, registered dietitian, and other healthcare providers before making significant changes to your diet or supplement regimen.
3. Potential Interactions:
Supplements can interact with medications, so it’s important to discuss all supplements with your doctor.
4. Quality and Safety:
Choose high-quality supplements from reputable brands.
Be aware that supplements are not regulated as strictly as medications.
5. Evidence-Based Approach:
Be wary of unsubstantiated claims and “miracle cures.”
Focus on evidence-based recommendations and work with your healthcare team to develop a personalized plan.

How to Manage MS Symptoms and Prevent Relapses
1. Physical Therapy
Physical therapy can help improve mobility, strength, and balance in people with MS.
A physical therapist can create a custom exercise program for you [19].
Benefits of physical therapy
- Better mobility
- Less muscle stiffness
- Improved balance and coordination
2. Occupational Therapy
Occupational therapy helps individuals with MS maintain their independence in daily activities.
This can include adaptive techniques and equipment to make tasks easier [20].
Benefits of Occupational Therapy
- Assisting with daily tasks
- Recommending adaptive equipment
- Providing strategies to save energy
3. Support Groups and Counseling
Support groups and counseling can offer emotional support and practical advice for managing MS.
Connecting with others who share a similar understanding can be highly beneficial [21].
How to find Support groups
- Local MS support groups
- Online forums and communities
- Professional counseling services
4. Regular Check-Ups
Regular check-ups with a neurologist are essential for tracking MS and adjusting treatment plans as needed [22].
What to Expect During Check-Ups
- Neurological exams
- MRI scans to monitor lesions
- Blood tests to check for medication side effects
Self-Care for MS

1. Adapting to Lifestyle Changes
Living with MS often means changing one’s lifestyle.
This might include modifying one’s home, work environment, or daily routine [23].
Practical Tips for Daily Living
- Install grab bars in the bathroom
- Use mobility aids if needed
- Plan rest periods throughout the day
2. Staying Active and Engaged
Staying active and engaged can help maintain physical and mental health.
Find activities that you enjoy and that fit your energy levels and abilities [24].
Activities to Consider
- Swimming or water aerobics
- Gentle yoga or stretching
- Hobbies like reading, painting, or gardening
Bottom Line
Early detection matters a lot.
Recognizing the signs, getting tested, and starting treatment can change your MS story.
Treating MS early results in fewer attacks, slower disease progression, and an improved quality of life.
So if something feels off, don’t ignore it. Talk to your doctor.
Which symptom caught your attention today?
I’m happy to hear from you. Leave your comment below and share this article.
Frequently Asked Questions
Q1: What are the first signs of MS?
The first signs of MS often include vision problems, numbness, tingling, and fatigue. These symptoms can appear suddenly and may be mistaken for other issues. If you notice these symptoms, it’s essential to consult a doctor.
Q2: How does MS affect your daily life?
MS can cause fatigue, muscle weakness, and difficulty walking, making daily tasks harder. Early treatment and lifestyle changes can help manage these symptoms and improve your quality of life.
Q3: Can diet help manage MS symptoms?
A balanced diet rich in fruits, vegetables, and omega-3 fatty acids can help reduce inflammation and support overall health. Supplements, such as vitamin D, may also be beneficial.
Q4: How important is early diagnosis of MS?
Early diagnosis is crucial for managing symptoms and slowing the progression of the disease. If you experience symptoms such as vision problems or numbness, consult a doctor immediately.
Q5: What lifestyle changes can help with MS?
Regular exercise, a healthy diet, stress management, and physical therapy can help manage MS symptoms. These changes can improve mobility, reduce fatigue, and enhance your overall well-being.
Q6: How long do optic neuritis symptoms last?
They usually improve in 2–4 weeks. However, some vision changes may persist for a longer period. Early steroid treatment can help speed recovery.
Q7: When should I get an MRI?
If you experience unexplained neurological symptoms, such as numbness, changes in vision, or weakness, doctors may order an MRI. It’s painless and quick.
References
- Browne P, Chandraratna D, Angood C, Tremlett H, Baker C, Taylor BV, et al. Atlas of Multiple Sclerosis 2013: A growing global problem with widespread inequity. Neurology [Internet]. 2014 Sep 9 [cited 2023 Nov 11];83(11):1022–4. Available from: https://www.neurology.org/lookup/doi/10.1212/WNL.0000000000000768
- Kobelt G, Thompson A, Berg J, Gannedahl M, Eriksson J, the MSCOI Study Group, et al. New insights into the burden and costs of multiple sclerosis in Europe. Mult Scler [Internet]. 2017 Jul [cited 2023 Nov 11];23(8):1123–36. Available from: http://journals.sagepub.com/doi/10.1177/1352458517694432
- Dobson R, Giovannoni G. Multiple sclerosis: a review. Eur J Neurol [Internet]. 2019 Jan [cited 2022 Nov 11];26(1):27–40. Available from: https://onlinelibrary.wiley.com/doi/10.1111/ene.13819
- Mollaoğlu M, Üstün E. Fatigue in multiple sclerosis patients. Journal of Clinical Nursing [Internet]. 2009 May [cited 2022 Nov 11];18(9):1231–8. Available from: https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2702.2008.02733.x
- Orton SM, Herrera BM, Yee IM, Valdar W, Ramagopalan SV, Sadovnick AD, et al. Sex ratio of multiple sclerosis in Canada: a longitudinal study. The Lancet Neurology [Internet]. 2006 Nov [cited 2022 Nov 11];5(11):932–6. Available from: https://linkinghub.elsevier.com/retrieve/pii/S147444220670581
- Baecher-Allan C, Kaskow BJ, Weiner HL. Multiple sclerosis: mechanisms and immunotherapy. Neuron [Internet]. 2018 Feb [cited 2022 Nov 11];97(4):742–68. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0896627318300461
- Ascherio A. Environmental factors in multiple sclerosis. Expert Review of Neurotherapeutics [Internet]. 2013 Dec [cited 2022 Nov 11];13(sup2):3–9. Available from: http://www.tandfonline.com/doi/full/10.1586/14737175.2013.865866
- Makhani N, Tremlett H. The multiple sclerosis prodrome. Nat Rev Neurol [Internet]. 2021 Aug [cited 2022 Nov 11];17(8):515–21. Available from: http://www.nature.com/articles/s41582-021-00519-3